A comprehensive suite of rejuvenation biotechnologies must include therapies that remove extracellular aggregates from aging cells and tissues. Of the biotechnologies in this class, immunotherapy against beta-amyloid (Aβ) is the furthest advanced along the clinical development pipeline.(1) The reasons for the pace of progress toward such therapies include the devastating impact of Alzheimer’s disease (to whose etiology and pathogenesis Aβ is generally accepted to be a major contributor) on victims and their families, but also its relatively recent designation as a distinct “disease,” and the widespread recognition of the rapidly-rising prevalence of Alzheimer’s disease due to the aging of global populations, since the biological aging process is by far the most important important driver of its clinical course.
The Progressive Unmasking of A Hidden Disease
At the other extreme is the very slow rate of progress to date toward the development of therapies against the aggregates responsible for age-related cardiac amyloidoses: senile systemic amyloidosis (SSA), caused by aggregated wild-type transthyretin (TTR), and isolated atrial amyloidosis (IAA), caused by aggregated atrial natriuretic peptide (ANP).(2,3) The prevalence of these cardiac amyloidoses is very low in middle age and early seniority (the youngest patient reported to have clinically-significant SSA was 57 years of age), but rises rapidly with each decade beginning at age 60, reaching 25% of persons ≥ 80 years.(2,3) Thus, the first cases of SSA are now beginning to appear in the postwar “Baby Boom” generation in the United States and elsewhere, and the prevalence and severity of the disease will rise further as they age; soon, the same will begin to occur elsewhere in the industrialized world, and soon thereafter in developing countries, the world undergoes a projected long period of global demographic aging.(10)
Cardiac amyloidosis infiltrates and disturbs the structural integrity of the heart muscle, as well as interfering with local cellular receptors and exerting direct cytotoxicity.(2) Even preclinical SSA exacerbates the morbidity of these diseases, for which it is often comorbid. And the disease is difficult to recognize: although the common clinical feature of age-related cardiac amyloidoses is a predominantly right-sided heart failure, the principle clinical signs and symptoms of SSA are nonspecific, and are commonly misdiagnosed as garden-variety congestive heart failure, cardiomyopathy, valvular heart disease, arrhythmia, or even coronary heart disease.(2)
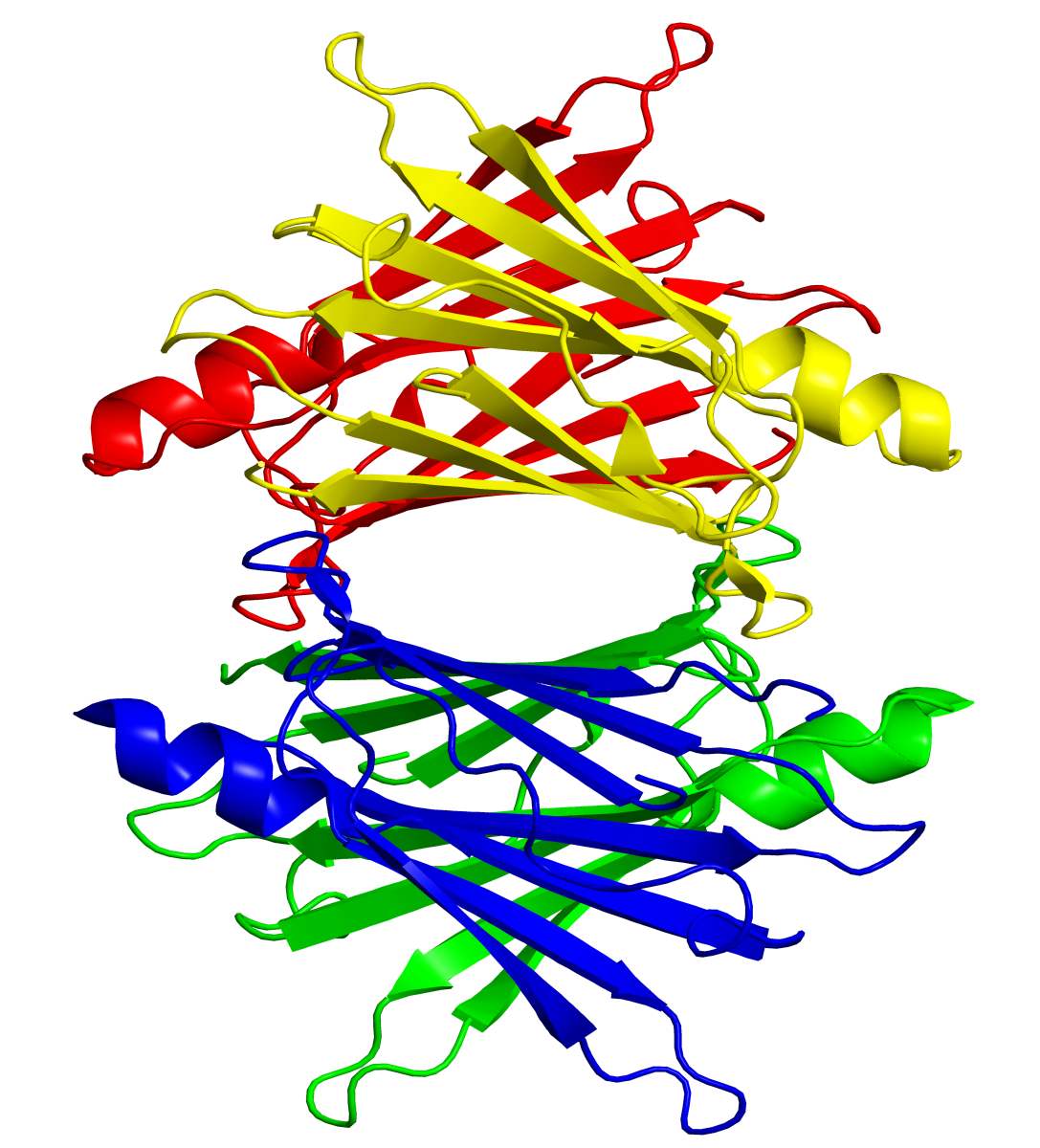
Transthyretin protein structure. Public domain image, Wikimedia and Tfoss.
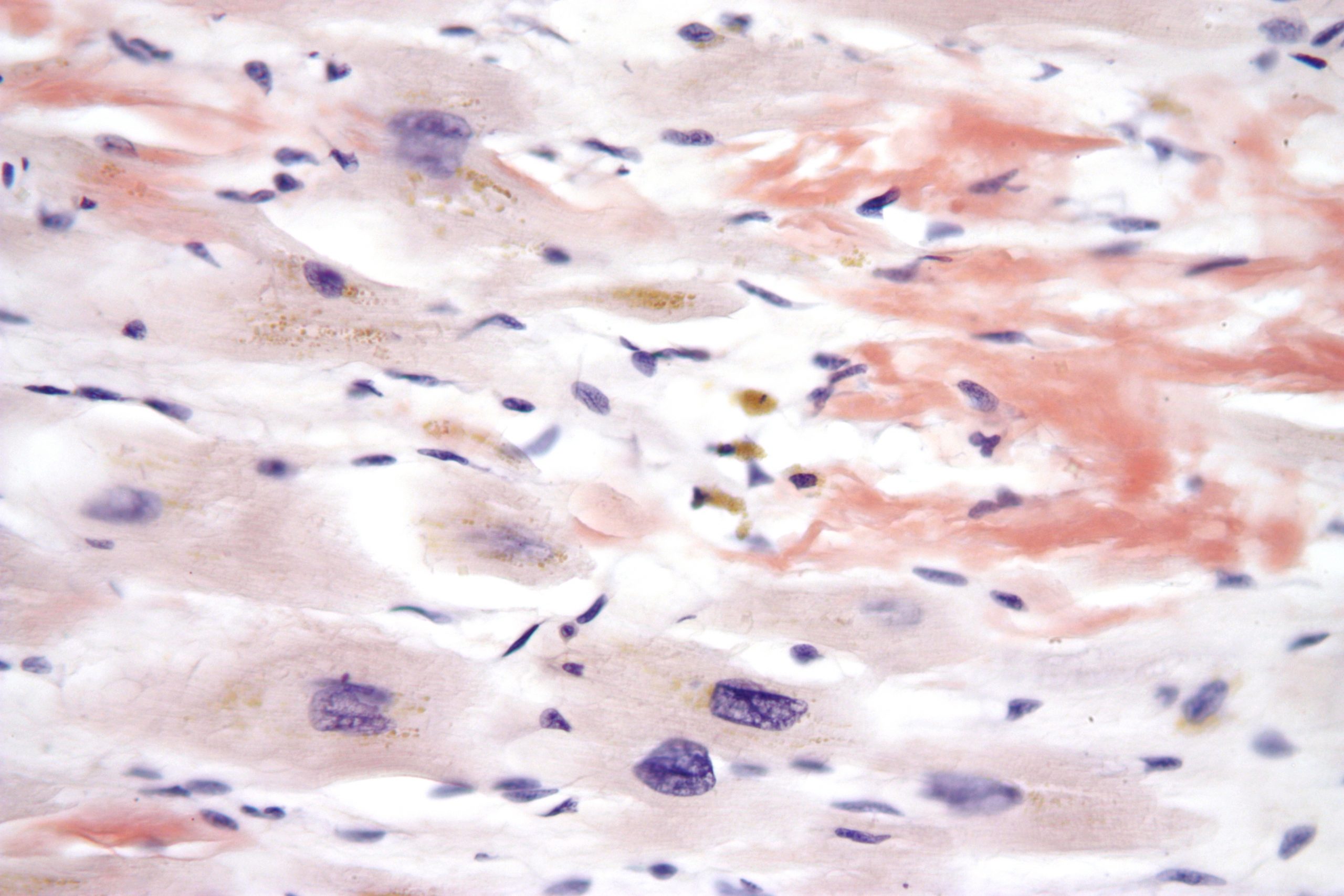
Micrograph of age-related cardiac amyloid. Licensed under the Creative Commons license (Wikimedia).
Unfortunately, while scintigraphy with 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid can be used to distinguish TTR-based cardiac amyloidosis from light-chain amyloidosis, the most reliable method of diagnosis today is through an invasive cardiac biopsy, followed by either staining with Congo red or binding with Thioflavin-T. Neither method suitable for routine clinical use, and clinicians are only likely to resort to either in the unlikely event that the clinician suspects cardiac amyloidosis rather than some more common cause of heart dysfunction. Misdiagnosis of the cause of the degeneration of patient hearts is therefore common, and leads to inappropriate medical therapy of what are actually only minor contributors to the underlying disease, resulting in treatment that is inefective at best and which, at worst, contributes to iatrogenic illness.
Even if SSA is correctly diagnosed, there is little that clinicians can do for patients today: there are currently no effective, disease-specific therapies available.
The full, ominous potential of SSA as a cause of age-related disability and death has been highlighted by the unique work of the Supercentenarian Research Foundation (SRF), who study the biology of human aging through extensive characterization of the health, disease, and causes of deaths of persons who have survived to ages ≥110 y. A key part of SRF’s scientific partnership with these Olympians of agingis the consensual autopsy of supercentenarians when they do ultimately die — critical work, because autopsies are only rarely performed in persons past the seventh decade of life, because of the ageist assumption that “people that old” “just die” of “natural causes” whose specific diagnosis is of low priority.
Instead, as early organizers Dr. Stephen Coles and Elliot Bergman realized in the early years of this century, the opposite is true: when a person has survived for so long without being taken from their loved ones by the most common diseases of aging, there is an enormous potential for us to learn about unguessed-at causes of age-related disability and death that will become core targets of future rejuvenation biotechnologies, as the prominent causes of disease and disability in their “normally”-aging cohorts today are successively defeated.
While only a limited number of such detailed pathological studies have yet been performed on centenarians, and just 11 with supercentenarians, results to date have been highly suggestive even as they are preliminary: “The most significant factor in the death of seven of these individuals was TTR senile systemic amyloidosis [my emphasis]. Supercentenarians have only a 50% chance of living for one year. Successful treatment of supercentenarians for TTR amyloidosis would improve their health, their quality of life, and their lifespan.”(4)
Thus, there is already a largely-unrecognized burden of SSA-related morbidity and mortality in the population today, both as a principle cause of death and disease and as a contributor to the total dysfunction of the aging cardiovascular system. And the situation will worsen globally over the course of the next 20 to 50 years, beginning in the industrialized world and the sequentially emerging in China, India, Mexico, the Middle East and beyond; ironically, this will be particularly so to the degree that other diseases are better-managed by progress in conventional medicine, or cured by rejuvenation biotechnology.
These features make the removal of wild-type TTR aggregates not only a concern of SRF as a research organization, but a key priority for SENS Foundation as a biomedical charity dedicated to accelerating the development of rejuvenation biotechnology. Accordingly, SENS Foundation has had an open request for proposals (RFP) for research toward the development of TTR-clearing therapies for several years now, and has approached several prominent researchers in the genetic amyloidosis field to submit applications for funding. Until recently, however, the Foundation had not received any strong proposals. But thanks to the efforts of SRF’s Stan Primmer, such a proposal has recently come together and the Foundation has been given the opportunity to fund it — and I am pleased to have the privilege of announcing that the proposal has been vetted, approved, and funded, and preliminary work will soon be under way.
September 2009: Leaks in the Therapeutic Pipeline
Because of his involvement with SRF, Primmer had long been very conscious of the clinical burden of SSA, and had surveyed the landscape of possible therapeutic approaches. But by the fall of 2009, as a result of his discussions with the present author and SENS Foundation Chief Science Officer Dr. Aubrey de Grey. he had become more conscious of the limitations of these approaches.(4)
First, very few of the therapies currently in development even for aggregates of mutant TTR would directly remove amyloid fibrils from the patient’s tissues. But because TTR amyloids accumulate progressively with age in the heart and other organs, therapies that merely retard or even prevent the formation or deposition of new aggregates do nothing to restore the healthy, normal functionality of the organ in persons whose cardiac function is already substantially impaired, or approaching the threshold of clinical significance. It is this feature of much of current, risk-factor-based medical research that limits its effectiveness against age-related disease, and which therefore needs to be replaced by an “engineering” heuristic focused on the actual removal, repair, replacement, or rendering harmless of the cellular and molecular damage of aging, in order to rejuvenate tissues instead of decelerating their age-related decline.
But there are also significant restrictions on the likely efficacy even of those few TTR-targeting therapies that were then in early-stage development that would (conceptually) remove existing TTR aggregates. Notably, all of them depended mechanistically upon the mobilization of the patient’s immune processes.(5-8) This implies that their ability to remove aggregates in would be significantly limited by the progressive decline in immune function that occurs as a result of the biological aging process, precisely in those persons most in need of therapy. This problem has in fact emerged with the Aβ-targeting immunotherapies in the most advanced stages of development, which are active and passive Aβ-targeting immunoglobulin G (IgG) vaccines. In the phase I trial of the active anti-Aβ vaccine AN1792, for example, serum anti-Aβ antibody titers were low, exceeding the secondarily-defined threshold of 1:1,000 in less than a quarter of AD patients, but it was only in such immunological responders that efficacy was demonstrated.(1) This low response was enhanced in the later Phase IIa trial by reformulation of the adjuvant, which increased the immunological response rate to nearly 60%, but generated a shift from a predominantly Th2 response to an inflammatory Th1 T-cell response. Unfortunately, this aggressive T-cell response led to the emergence of meningoencephalitis in ~6% of patients, leading to the early cessation of the trial.(1) In Phase I testing, passive vaccination with bapineuzumab has caused vascular microhaemorrhages in a minority of apolipoprotein E ε4 carriers, thought to be caused by deposition of IgG-bound Aβ in the cerebral vasculature.(1)
A similar constraint was in evidence in preclinical testing of a TTR-targeting antibody (in an animal model of a cross-reacting amyloidosis) when it included aged (>18 months) and immunodeficient (SCID) mice as a comparison to the standard cohort of young animals.(5) In young animals, injected antibodies rapidly bound to amyloid tumors, leading to rapid fibrillogenic tumor dissolution. Detailed study of this process revealed extensive infiltration of aggregates by neutrophils shortly after antibody opsonization, which they hypothesized to result from attraction and activation of neutrophils through their Fcγ receptors and consequent release of proteolytic enzymes and/or reactive oxygen species. But in aged and immunodeficient mice, amyloid dissolution was still incomplete at the end of the 3 mo study. (5)
An ideal therapy would therefore not depend on the patient’s immune status for effectiveness or safety, but would be in itself sufficient for therapeutic benefit.
As an additional concern, all TTR-targeting immunotherapies currently in preclinical testing are relatively nonspecific, either binding to off-target molecules, or only binding to the mutant TTR protein and its aggregates to the neglect of the aggregates of wild-type protein underlying SSA.
Thanks to a dinner meeting that SRF’s Primmer enjoyed with a key researcher during their attendance at the Fourth SENS Scientific Conference (SENS4), the construction of a new, robust pipeline is now underway.
Project: Develop Catalytic Antibodies Against Wild-Type TTR
Primmer had been seated at dinner at a table with Dr. Sudhir Paul, who was presenting the work that he and his group at the Chemical Immunology Research Center at the University of Texas-Houston Medical School at the meeting. As we reviewed in a previous posting, Paul’s group have made significant progress with a promising novel approach to Aβ immunotherapy: catalytic Aβ-targeting antibody fragments that cleave, rather than sequester, these pathological aggregates.
In the course of conversation, Primmer mentioned the SRF’s focus on the biomedical challenge of developing new diagnostics and therapies against TTR, for the health of both the extreme survivors with whom he works and the general aging population. Primmer had missed Dr. Paul’s presentation, and Paul did not interject at the time to outline his work with Aβ. But Paul later realized the potential to extend his own methods, developed while researching his Aβ-targeting antibody fragments, to the development of similar cleaving catalysts against the TTR amyloids underlying SSA.
As reviewed in that earlier posting, this approach in principle offers multiple advantages in Alzheimer’s disease and brain aging relative to other Aβ immunotherapies, in terms of both efficacy and safety. What Paul now came to realize was that these same features, translated into a catalytic TTR-targeting immunotherapy, would in principle overcome all the obvious limits to those currently in development. They would remove existing aggregates, rather than retarding their further accumulation; exploitation of Paul’s protocols would allow them to enrich for highly specific antibody fragments with high catalytic activity; they are catalytic in their activity, reducing the quantity and frequency of injected antibody required to achieve aggregate clearance; they hydrolyze the aggregates, rather than simply sequestering them for later passive degradation or excretion, and do not form stable antibody-Aβ intermediates, avoiding potential side-effects of monomer mobilization and interaction of complexes with surrounding tissues; and they do not rely on patients’ immune response for efficacy, eliminating the major possible cause of reduced efficacy in the biologically aged patient and the risk-fraught necessity to induce a strong inflammatory response for their effectiveness.(9)
Listening to Paul, Primmer quickly recognized the high potential of this approach. But it would be difficult to identify suitable patients for clinical trials, or to ensure that even an approved therapy would reach the patients who need it most, if there remained no effective, noninvasive, in vivo diagnostic method for SSA, especially at relatively early ages. By happy coincidence, Paul was already scheduled to speak at the first International Forum on Immunoglobulin Research at Fort Lauderdale, FL that November, as was Dr. Brian O’Nuallain. Primmer was already familiar with the work of Drs. Alan Solomon and O’Nuallain on TTR-targeting antibodies, and the three arranged to meet at the conference, to discuss the possibility of a collaboration. The product of these conversations was a draft proposal for a four-phase research and development project:
Phase 1 will consist of in vitro generation of two separate sets of monoclonal antibodies: (a) antibodies that bind to TTR amyloid for subsequent diagnostic use, and (b) catalytic antibodies that can directly destroy TTR amyloid. … Phase 2 will consist of studies in an animal model of TTR amyloidosis to determine the safety and efficacy of the potential diagnostic and therapeutic antibodies discovered in Phase 1. Phase 3 will involve clinical trials on the diagnostic and therapeutic potential of the novel antibodies for comparatively young human subjects who develop amyloidosis due to mutation(s) in the TTR molecule. Initial testing of the methodology in the younger cohort is designed to avoid risk to the uniquely fragile group consisting of supercentenarians. Phase 4 will then serve to apply the results of previous research to volunteer supercentenarians in order to improve their health and extend their lives beyond what they would otherwise be expected to live.(4)
The initial phases of the project would be divided according to the expertise of the respective researchers, with O’Nuallain largely responsible for the initial development of a diagnostic binding antibody against wild-type TTR aggregates and later testing in his existing animal models, and Paul for the isolation, purification, and pharmacological optimization of the catalytic cleavage antibody fragment. Along with the proposal came anticipated research budgets for the first two phases, with estimates for the remaining phases to be developed based on their fruits.
The critical issue, of course, was securing funding for such a novel project on an underprioritized age-related disease. Aware of SENS Foundation’s recognition of the critical-path priority of such research in the development of comprehensive rejuvenation biotechnology, Primmer submitted the preliminary proposal to CSO de Grey. Following further clarification and negotiation of the draft protocol, and consultation with SENS Foundation’s Research Committee, all parties agreed upon a final research plan for Phase I, and the $150 000 research investment was approved by SENS Foundation and disbursed to the researchers.
We are delighted to have such a strong project underway, in the hands of recognized experts in the field, and I am personally grateful for the critical networking done by Primmer and the Supercentenarian Research Foundation to bring the proposal together, and proud of SENS Foundation’s role as funder of this promising project. TTR-based senile cardiac amyloidosis is an underdiagnosed and heretofore-untreatable disease that is prevalent in the aging population and poised to become a widespread medical problem with the aging of the global population and the improved treatment of more familiar age-related diseases. We will watch the progress of this latest funded research project with keen anticipation, and look cautiously forward to the ultimate culmination of the preclinical groundwork in a therapy for human patients.
References
1. Lemere CA, Masliah E. Can Alzheimer disease be prevented by amyloid-beta immunotherapy? Nat Rev Neurol. 2010 Feb;6(2):108-19. PubMed PMID: 20140000; PubMed Central PMCID: PMC2864089.
2. Kholová I, Niessen HW. Amyloid in the cardiovascular system: a review. J Clin Pathol. 2005 Feb;58(2):125-33. Review. PubMed PMID: 15677530; PubMed Central PMCID: PMC1770576.
3. Steiner I, Hájková P. Patterns of isolated atrial amyloid: a study of 100 hearts on autopsy. Cardiovasc Pathol. 2006 Sep-Oct;15(5):287-90.
4. Primmer SR, Paul S, O’Nuallain B. Research project to extend lives of supercentenarians by diagnosing and treating transthyretin amyloidosis. Unpublished MS, Supercentenarian Research Foundation. 2010 Mar 25.
5. Hrncic R, Wall J, Wolfenbarger DA, Murphy CL, Schell M, Weiss DT, Solomon A. Antibody-mediated resolution of light chain-associated amyloid deposits. Am J Pathol. 2000 Oct;157(4):1239-46. PubMed PMID: 11021828; PubMed Central PMCID: PMC1850152.
6. Terazaki H, Ando Y, Fernandes R, Yamamura K, Maeda S, Saraiva MJ. Immunization in familial amyloidotic polyneuropathy: counteracting deposition by immunization with a Y78F TTR mutant. Lab Invest. 2006 Jan;86(1):23-31. PubMed PMID: 16357867.
7. Goldsteins G, Persson H, Andersson K, Olofsson A, Dacklin I, Edvinsson A, Saraiva MJ, Lundgren E. Exposure of cryptic epitopes on transthyretin only in amyloid and in amyloidogenic mutants. Proc Natl Acad Sci U S A. 1999 Mar 16;96(6):3108-13. PubMed PMID: 10077645; PubMed Central PMCID: PMC15903.
8. Costa PM, Teixeira A, Saraiva MJ, Costa PP. Immunoassay for transthyretin variants associated with amyloid neuropathy. Scand J Immunol. 1993 Aug;38(2):177-82. PubMed PMID: 8394031.
9. Paul S, Planque S, Nishiyama Y. Beneficial catalytic immunity to Abeta peptide. Rejuvenation Res. 2010 Apr-Jun;13(2-3):179-87. Review. PubMed PMID: 20370602.
10. Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008 Feb 7;451(7179):716-9.



