Hello, my name is Connor Crowley, and I am a junior studying biochemistry at Wake Forest University. I have always been extremely interested in the incredible possibilities of regenerative medicine and was thrilled to hear that I was selected as a SRF-WFIRM research scholar. While I don’t believe that I have a specific moment in time that definitively pushed me towards regenerative medicine, I do believe that we have all seen the devastating effects that aging can have on our loved-ones, friends, and family members. Throughout my short 20-year life I have watched my grandfather’s life transform, all due to the effects of aging. When I was younger, he always played golf and baseball beside me. When I was a teenager, he was still by my side, but solely as an instructor as years of lifeguarding and tennis had made his joints tender and left him with bad arthritis. Today, I see my grandfather bedridden and no longer able to watch me play any of the sports he used to love. We regard all of this as life and simply jot it down as a part of the aging process, while we scramble desperately to treat its effects. Throughout this scramble we pump hundreds of thousands of dollars into our treatment yet completely overlook the true cause of this: aging. Writing it off as untreatable for far too many generations, we have completely ignored the possibilities of regenerative medicine to work as an anti-aging agent. Through my research with the SENS Research Foundation and Wake Forest Institute for Regenerative Medicine (WFIRM), I hope to not only make advances in the lab but also help advance the acceptance and viability of regenerative medicine in the future of healthcare.
Prior to my selection for the SRF-WFIRM research scholar program, I worked in the laboratory of Dr. Patricia Dos Santos and analyzed a class of enzymes known as cysteine desulfurases. These enzymes are aptly named as their main function is to cleave sulfur from the amino acid cysteine. Through the cleavage and mobilization of sulfur, cysteine desulfurases incorporate sulfur into iron-sulfur cofactors and aid the production of the sulfur bridges that hold together many of the essential proteins that our body uses each and every day. A better understanding of these poorly studied proteins could improve the targeting and specificity of future therapeutics, and this incredible pertinence to our body’s biological systems is one of the main reasons I joined Dr. Dos Santos’ lab. Under the mentorship of Dr. Bruna Selbach, at the time a graduate student in the Dos Santos lab, I analyzed the kinetics and mechanistic function of several desulfurase enzymes. One highlight of this work was my characterization of the poorly understood NifS enzyme. Through a combination of enzymatic assays and HPLC analysis, I was able to determine the Km and Kkat and gained a better understanding of NifS’s role in the formation of iron-sulfur clusters. Furthermore, these results, combined with a mechanistic analysis of NifS, suggested ways we could regulate the NifS pathway.
As an SRF-WFIRM research scholar in the laboratory of Dr. Graca Almeida-Porada, I plan to study mesenchymal/stromal cells (MSCs) as a potential treatment and hopeful cure to inflammatory bowel disease (IBD). The choice of MSCs as a potential treatment of IBD is largely two-fold. First, it is well known that MSCs are able to selectively target areas of inflammation and injury following systematic infusion. Once localized at the area of inflammation, MSCs have demonstrated high levels of engraftment and have, furthermore, proven to initiate the process of tissue repair through the release of soluble factors that promote healing of the surrounding area. The second advantage of MSCs as a treatment of IBD is the ability to reduce inflammation and hyper-immune response surrounding the injury. Both of these unique abilities make MSCs a perfect candidate for IBD treatment, particularly since they address two of the main symptoms of the disease.
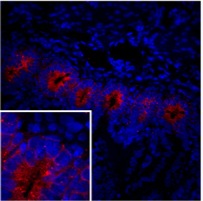
Figure 1. Mushashi-1+ cells within the intestinal crypts.
Despite these two clear advantages and many successes observed in preliminary animal clinical trials, the effectiveness of MSCs to treat IBD in humans has yet to be conclusively proven. We suspect that the severe pro-apoptotic environment of the IBD gut may be the reason for this discrepancy. Throughout this semester, I plan to modify MSC’s to help them survive this harsh environment and engineer cells that are less prone to the allogeneic immune response. We hope these adjustments will increase the binding of the MSCs to areas of inflammation and through the natural repair mechanisms of these cells provide a viable over-the-counter option for the treatment of IBD.
Future Plans:
I plan to use my research with Dr. Almeida-Porada as the subject for my senior thesis work and graduate with honors from Wake Forest University in the spring of 2015. After graduation, I hope to attend medical school to achieve my ultimate goal of becoming a flight surgeon in the Air Force. That would combine the two things I have always wanted to do in my life: help others and serve my country. I cannot think of a better way to live-out the rest of my life than helping our country’s soldiers recover from their injuries.


