John is currently a senior at Vassar College majoring in Biology. Since 2011, he has been studying the neuroprotective effects of hormones released following traumatic brain injury in the laboratory of Dr. Kelli A. Duncan. During his 2013 SENS Research Foundation (SRF) Summer Internship Program, he joined the laboratory of Dr. Graca Almeida-Porada at the Wake Forest Institute for Regenerative Medicine and helped develop a stem-cell based therapy for the treatment of inflammatory bowel disease (IBD) in mouse models.
Stem cell-based therapy for the treatment of inflammatory bowel disease (IBD)
Inflammatory bowel disease is characterized by intestinal inflammation, which causes severe damage to the tissue of the intestinal lining. The precise cause of IBD remains uncertain. However, evidence suggests that dysregulation of the immune system plays a role in the autoimmune response that leads to the inflammation that characterizes IBD. Mesenchymal stromal cells (or MSCs) are cells which differentiate into multiple tissue types and have been shown to reduce local inflammation, decrease the immune response, and counteract the chemotactic signals released to recruit immune cells to the site of inflammation. It was therefore hypothesized that MSCs may be an effective therapy for IBD. However, clinical trials have demonstrated that MSC infusions were only effective in 30% of IBD patients. Furthermore, animal model studies have demonstrated that the limited tendency of MSCs to graft to the intestine may have been the limiting factor.
Previous work by the Almeida-Porada lab indicates that endothelial progenitor cells home promptly to the intestine. Therefore, my summer project sought to explore whether a cell-based therapy using a combination of both MSCs and endothelial cells (EC) would be an effective treatment for IBD. We hypothesized that this approach could be the ideal platform to decrease inflammation/apoptosis, reset the immunomodulatory immune response, normalize vascularization, repopulate the intestinal stem cell pool, and generate differentiated intestinal cells.
Therefore , I isolated and characterized mesenchymal stromal cells and endothelial cells from human umbilical cord tissue. Then, I utilized flow cytometry and immunofluorescent double-staining to characterize these cells, and show that our cells are expressing molecules necessary for homing and immunomodulation
These results also lay the groundwork for future experiments to evaluate the effectiveness of cord tissue-derived MSC and EC cell therapy in a T-cell transfer murine model of IBD that I helped develop.
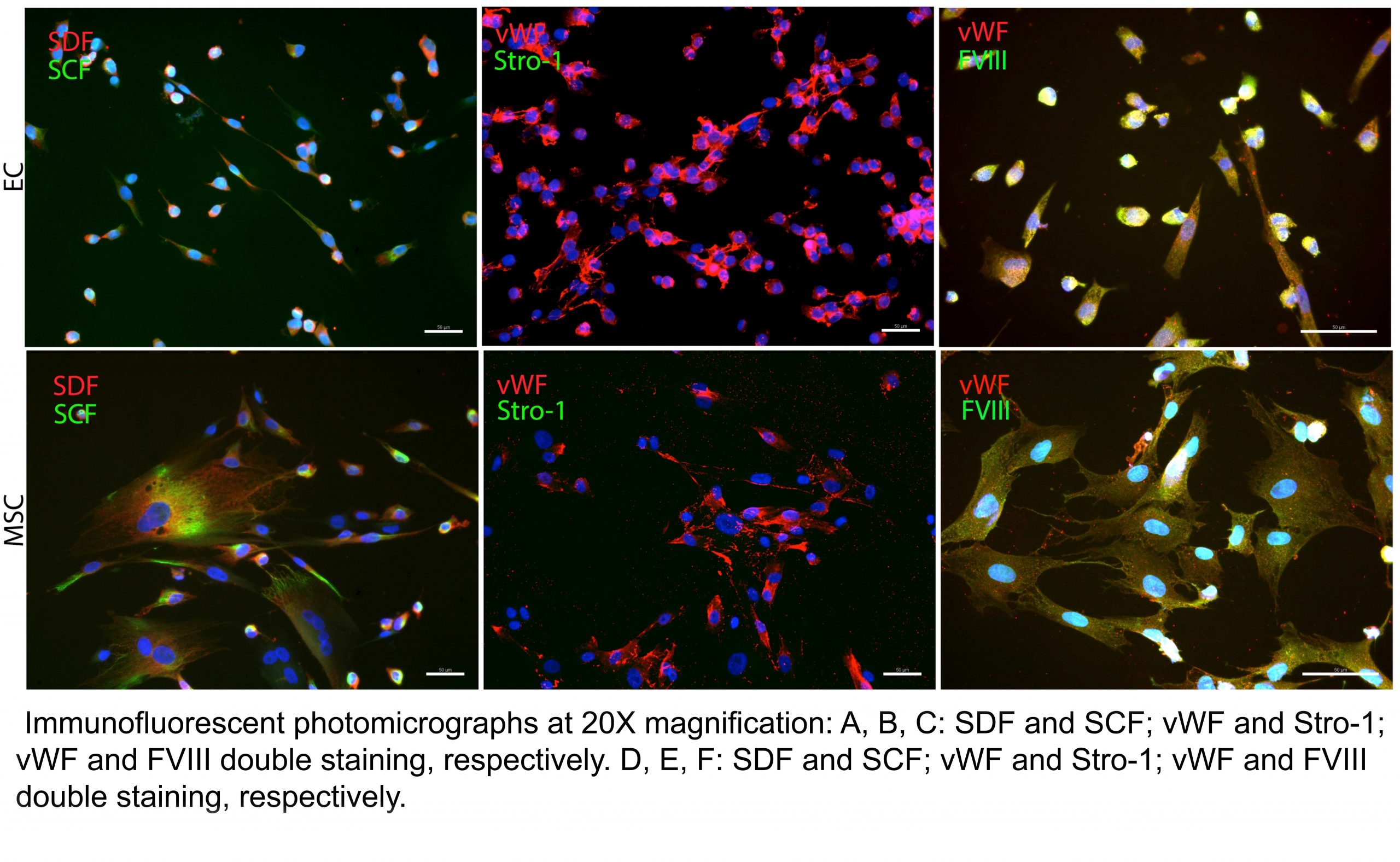
Figure 1.
Future Plans:
John presented his findings at the SENS6: Reimagine Aging Conference held at the University of Cambridge in September 2013. He will complete his undergraduate studies at Vassar College this semester and hopes to pursue postgraduate studies in either an MD or MD/PhD program.


